Conditions
Drugs
Insurances
TCM
Research
About Us
Contact Us
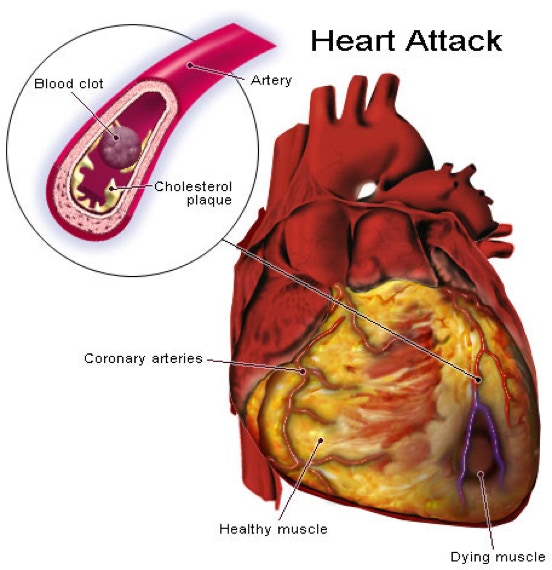
What is a heart attack (myocardial infarction)?
A heart attack, or myocardial infarction, happens when one or more regions of the heart muscle experience a severe or prolonged lack of oxygen caused by blocked blood flow to the heart muscle.
The blockage is often a result of atherosclerosis. This is a buildup of plaque composed of fat deposits, cholesterol, and other substances. When a plaque ruptures, a blood clot quickly forms. The blood clot is the actual cause of the heart attack.
If the blood and oxygen supply is cut off, muscle cells of the heart begin to suffer damage and start to die. Irreversible damage begins within 30 minutes of blockage. The result is dysfunction of the heart muscle in the area affected by the lack of oxygen or cell death.
What are the risk factors for heart attack?
There are 2 types of risk factors for heart attack, including the following:
Inherited (or genetic)
Acquired
Inherited or genetic risk factors are risk factors you are born with that cannot be changed, but can be improved with medical management and lifestyle changes.
Acquired risk factors are caused by activities that we choose to include in our lives that can be managed through lifestyle changes and clinical care.
Inherited (genetic) factors: Who is most at risk?
The following are those most at risk:
People with inherited hypertension (high blood pressure)
People with inherited low levels of HDL (high-density lipoproteins), high levels of LDL (low-density lipoprotein) blood cholesterol or high levels of triglycerides
People with a family history of heart disease (especially with onset before age 55)
Aging men and women
People with type 1 diabetes
Women, after the onset of menopause. Generally, men are at risk at an earlier age than women. After the onset of menopause, women are equally at risk.
Acquired risk factors: Who is most at risk?
The following are those most at risk:
People with acquired hypertension (high blood pressure)
People with acquired low levels of HDL (high-density lipoproteins), high levels of LDL (low-density lipoprotein) blood cholesterol, or high levels of triglycerides
Cigarette smokers
People who are under a lot of stress
People who drink too much alcohol
People who lead a sedentary lifestyle
People overweight by 30% or more
People who eat a diet high in saturated fat
People with type 2 diabetes
A heart attack can happen to anyone. It is only when we take the time to learn which of the risk factors apply to us, specifically, can we then take steps to eliminate or reduce them.
Managing heart attack risk factors
Managing your risks for a heart attack begins with:
Examining which of the risk factors apply to you, and then taking steps to eliminate or reduce them.
Becoming aware of conditions like hypertension or abnormal cholesterol levels. These may be "silent killers."
Modifying risk factors that are acquired (not inherited) through lifestyle changes. Talk with your healthcare provider as the first step in starting right away to make these changes.
Talking with your healthcare provider soon to determine if you have risk factors that are genetic or inherited and cannot be changed. They can be managed medically and through lifestyle changes.
What are the warning signs of a heart attack?
The following are the most common symptoms of a heart attack. However, each individual may experience symptoms differently. Symptoms may include:
Severe pressure, fullness, squeezing, pain and/or discomfort in the center of the chest that lasts for more than a few minutes
Pain or discomfort that spreads to the shoulders, neck, arms, or jaw
Chest pain that increases in intensity
Chest pain that is not relieved by rest or by taking nitroglycerin
Chest pain that happens with any or all of the following (additional) symptoms:
Sweating, cool, clammy skin, and/or paleness
Shortness of breath
Nausea or vomiting
Dizziness or fainting
Unexplained weakness or fatigue
Rapid or irregular pulse
Although chest pain is the key warning sign of a heart attack, it may be confused with indigestion, pleurisy, pneumonia, costochondritis (inflammation and tenderness of the cartilage that attaches the front of the ribs to the breastbone), heartburn, or other disorders.
The symptoms of a heart attack may resemble other medical conditions or problems. Always talk with your healthcare provider for a diagnosis.
Responding to heart attack warning signs
If you or someone you know exhibits any of the above warning signs, act immediately. Call 911, or your local emergency number.
Treatment for a heart attack
The goal of treatment for a heart attack is to relieve pain, preserve the heart muscle function, and prevent death.
Treatment in the emergency department may include:
Intravenous therapy, such as nitroglycerin and morphine.
Continuous monitoring of the heart and vital signs.
Oxygen therapy improves oxygenation to the damaged heart muscle.
Pain medicine decreases pain, and, in turn, decreases the workload of the heart, thus, the oxygen demand of the heart decreases.
Cardiac medicine, such as beta-blockers, promote blood flow to the heart, improve the blood supply, prevent arrhythmias, and decrease heart rate and blood pressure.
Fibrinolytic therapy is the intravenous infusion of a medicine that dissolves the blood clot, thus, restoring blood flow.
Antithrombin or antiplatelet therapy, such as aspirin or clopidogrel, is used to prevent further blood clotting.
Antihyperlipidemics are medicines used to lower lipids (fats) in the blood, particularly Low Density Lipid (LDL) cholesterol. Statins are a group of antihyperlipidemic medicines, and include simvastatin, atorvastatin, and pravastatin, among others. Bile acid sequestrants—colesevelam, cholestyramine, and colestipol—and nicotinic acid (niacin) are 2 other types of medicines that may be used to reduce cholesterol levels.
Additional procedures to restore coronary blood flow may be used. Those procedures include:
Coronary angioplasty. With this procedure, a balloon is used to create a bigger opening in the vessel to increase blood flow. This is often followed by the insertion of a stent into the coronary artery to help keep the vessel open. Although angioplasty is performed in other blood vessels elsewhere in the body, percutaneous coronary intervention (PCI) refers to angioplasty in the coronary arteries to permit more blood flow into the heart. PCI is also called percutaneous transluminal coronary angioplasty (PTCA). There are several types of PTCA procedures, including:
Balloon angioplasty. A small balloon is inflated inside the blocked artery to open the blocked area.
Coronary artery stent. A tiny coil is expanded inside the blocked artery to open the blocked area and is left in place to keep the artery open.
Atherectomy. The blocked area inside the artery is cut away by a tiny device on the end of a catheter.
Laser angioplasty. A laser used to "vaporize" the blockage in the artery.
Coronary artery bypass. Most commonly referred to as simply "bypass surgery" or CABG (pronounced "cabbage"), this surgery is often performed in people who have angina (chest pain) and coronary artery disease (where plaque has built up in the arteries). During the surgery, a bypass is created by grafting a piece of a vein above and below the blocked area of a coronary artery. This enables blood to flow around the obstruction. Veins are usually taken from the leg, but arteries from the chest or arm may also be used to create a bypass graft. Sometimes, multiple bypass surgeries are necessary to restore bloodflow to all areas of the heart.