Doctors
Institutions
Conditions
Drugs
Insurances
TCM
Research
About Us
Contact Us
What Is Mitral Valve Prolapse?
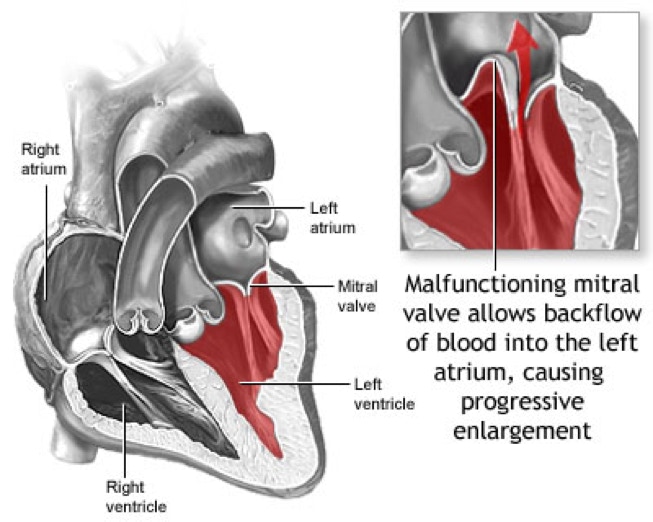
The mitral valve consists of two flaps, or leaflets, that separate the left heart's atrium (upper chamber) and ventricle (lower chamber). In a healthy heart, as the heart relaxes and the mitral leaflets open and blood flows from atrium into ventricle and then, when the heart squeezes pumps blood out to the body, the mitral leaflets close and form a tight seal so that blood does not leak backward.
Mitral valve prolapse (MVP) is also sometimes known as myxomatous mitral valve disease or floppy valve syndrome. It affects 2-3% of the population, making it one of the most common congenital heart conditions. In MVP one or both of the leaflets has excess tissue. This abnormality, which is present from birth, causes the leaflet(s) to sag and bow backward into the left atrium each time the heart contracts. It usually prevents the leaflets from closing properly, which leads to mitral regurgitation (blood leaking backward from the left ventricle into the left atrium). In MVP, extra strain on the chordae (the thin strings in the ventricle that support the valve) can, over time, cause the chordae to snap or break, leading to worsening regurgitation.
Mild mitral regurgitation is well tolerated and should not cause any significant problems. Moderate to severe mitral regurgitation, however, increases the heart's workload and thus over time, may lead to complications such as:
Enlargement of the heart
Weakness of the heart muscle
Atrial fibrillation
Pulmonary hypertension
Fortunately, being diagnosed with MVP is not a cause for alarm. Most people with MVP lead normal, symptom-free lives with no lifestyle restrictions.
Sometimes, particularly when mitral regurgitation is severe, surgery may be necessary to correct the MVP. By closely monitoring the disease and watching for signs of its progression, your doctor can be proactive in determining if and when surgery is necessary. When surgery is performed before the left ventricle is significantly compromised, outcomes generally are quite positive.
Risk Factors
Unlike other kinds of heart disease, MVP is an abnormality from birth and is not associated with smoking, diet or lifestyle. In a minority of cases, MVP is associated with connective tissue disorders, such as Marfan syndrome, which can affect both the mitral valve and the aorta.
Symptoms
Many people with MVP have no symptoms. Some people may experience symptoms such as:
Fast or irregular heart beat
Shortness of breath
Chest pain
Fatigue
Dizziness or lightheadedness
Having symptoms does not always correlate with how much mitral regurgitation is present (how much the valve leaks) or the seriousness of MVP. Some people may have symptoms but cardiac testing shows the valve does not leak very much. Having symptoms without significant regurgitation may cause a person to worry, but is not dangerous, life-threatening or require any treatment at all.
People with severe mitral regurgitation may begin to experience shortness of breath, especially with exertion, and this could signal the need for surgery. In rare instances, MVP with significant regurgitation can lead to overt congestive heart failure and even sudden death, if left untreated.
If you have MVP, it is therefore very important to have a doctor evaluate you on a regular basis.
Diagnosis
During a physical examination, your doctor may suspect MVP upon detecting abnormal heart sounds (click and/or murmur) with a stethoscope. Other tests used to evaluate MVP may include:
Echocardiogram
Transesophageal echocardiogram
Cardiac catheterization
Cardiac MRI
Most patients who have a murmur should have an echocardiogram (ultrasound of the heart), which is the primary test for diagnosing MVP and establishing its severity.
The echocardiogram is also used to track the progression of MVP. If the condition has reached an advanced stage, your doctor may perform a cardiac catheterization (in which pressures inside your heart are measured and digital images are used to identify narrowing or blockage in the heart arteries) to determine if surgery is needed.
A transesophageal echocardiogram or, more recently, a real-time three dimensional (3D) transesophageal echocardiogram, may be helpful to give doctors a more detailed understanding of the anatomy of the mitral valve and help determine whether it can be repaired surgically. Be sure to ask if these advanced imaging technologies are available at your hospital.
Treatment
While MVP is present at birth, it often is not diagnosed until much later in life. In its earlier stages, the condition simply requires ongoing monitoring. If it progresses, medical or surgical treatments may be necessary.
Monitoring
Most people with MVP do not require medicines or surgery, but need to be followed regularly by their doctor to monitor for changes in the valve’s function. Additional tests, such as echocardiograms, may need to be repeated from time to time.
Medical Treatments
No medications can prevent MVP from occurring or progressing. However, some medications may be helpful in managing symptoms and preventing complications.
For example:
Diuretics may relieve symptoms associated with MVP or potentially slow the impact of significant regurgitation on the left ventricle
Blood pressure-lowering drugs may reduce the impact of mitral regurgitation
Blood thinners may help treat atrial fibrillation, which sometimes accompanies the MVP with significant mitral regurgitation
Surgical Treatments
The underlying problem in MVP is mechanical in nature, in that the mitral valve does not close properly. If the valve has become severely compromised and is leaking badly, surgery is the only effective solution.
A variety of tactics can be used to preserve the existing valve and prevent regurgitation, such as:
Removing excess tissue in the mitral leaflets
Repairing or replacing broken chordae
Annuloplasty (inserting a cloth-covered ring around the outside of the mitral valve to support it)
Surgical replacement of the valve may be appropriate if the existing valve has been compromised by endocarditis (a valve infection) or if the regurgitation is caused by rheumatic, radiation or ischemic heart disease.
Mechanical valves are typically are used in people under 70 years of age because they tend to be durable. However, patients with a mechanical valve must take blood thinner pills for the rest of their lives to prevent formation of blood clots on the valve that could lead to stroke
Tissue valves, made from cow or pig heart tissue, are typically are used in people 70 years and older. These valves may eventually wear out and need replacement, but they do not require patients that take a blood thinner
Mitral valve repair and replacement both require open surgery and have a recovery time of 2-3 months. However, repair has many advantages compared with replacement, including:
Higher long-term survival rates
Better preservation of heart function
Lower risk of stroke, valve infection and other complications
If you are considering surgery to address MVP, make sure your surgeon is highly experienced in repairing valves.
Most mitral valve surgery requires a traditional incision, although in certain cases minimally invasive techniques, including robotic-assisted surgery, may be an option. In addition, catheter-based therapies for valve repair are emerging but still in the investigational stage.