Doctors
Institutions
Conditions
Drugs
Insurances
TCM
Research
About Us
Contact Us
What is alcohol-induced liver disease?
Alcohol-induced liver disease is common, but can be prevented. There are 3 types. Many heavy drinkers progress through these 3 types over time:
Fatty liver. Fatty liver is the build-up of fat inside the liver cells. It leads to an enlarged liver. It’s the most common alcohol-induced liver problem.
Alcoholic hepatitis. Alcoholic hepatitis is an acute inflammation of the liver. There is death of liver cells, often followed by permanent scarring.
Alcoholic cirrhosis. Alcoholic cirrhosis is the destruction of normal liver tissue. It leaves scar tissue in place of the working liver tissue.
The liver is a large organ that sits up under the ribs on the right side of the abdomen (belly). The liver:
Helps filter waste from the body
Makes bile to help digest food
Stores sugar that the body uses for energy
Makes proteins that work in many places in the body, for example, proteins that cause blood to clot
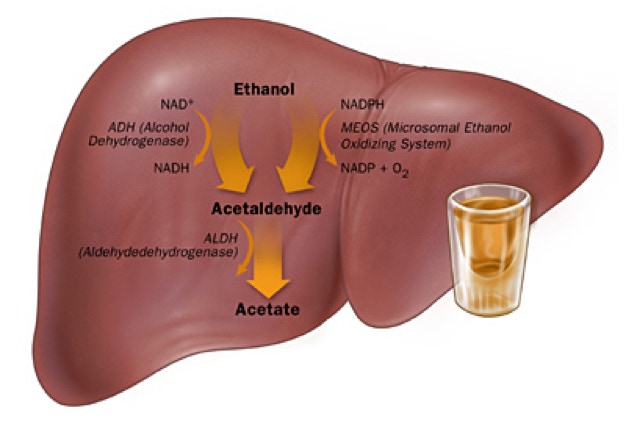
What causes alcohol-induced liver disease?
Alcohol-induced liver disease is caused by heavy use of alcohol. The liver’s job is to break down alcohol. If you drink more than it can process, it can become badly damaged.
Fatty liver can happen in anyone who drinks a lot. Alcoholic hepatitis and alcoholic cirrhosis are linked to the long-term alcohol abuse seen in alcoholics.
Doctors don’t know why some people who drink alcohol get liver disease while others do not. Research suggests there may be a genetic link, but this is not yet clear.
What are the symptoms of alcohol-induced liver disease?
The effects of alcohol on the liver depend on how much and how long you have been drinking alcohol. These are the most common symptoms and signs:
Fatty liver
Often causes no symptoms
Build-up of fat inside the liver cells enlarges the liver, causing upper abdominal (belly) discomfort on the right side
Tiredness and weakness
Weight loss
Alcoholic hepatitis
Pain over the liver
Fever
Weakness
Nausea and vomiting
Appetite loss
Yellowing of the skin and eyes (jaundice)
Alcoholic cirrhosis, all of the symptoms of alcoholic hepatitis and
Portal hypertension (increased resistance to blood flow through the liver)
Enlarged spleen
Poor nutrition
Bleeding in the intestines
Ascites (fluid build-up in the belly)
Kidney failure
Confusion
Liver cancer
The symptoms of alcohol-induced liver disease may look like other health problems. Always see a doctor for a diagnosis.
How is alcohol-induced liver disease diagnosed?
Your doctor will do a complete health history and physical exam. Other tests used to diagnose alcohol-induced liver disease may include:
Blood tests. Including liver function tests, which show whether the liver is working the way it should.
Liver biopsy. This involves removing small tissue samples from the liver with a needle or during surgery. These samples are checked under a microscope to find out the type of liver disease.
Ultrasound. This test uses high frequency sound waves to create a picture of the organs.
Computed tomography (CT) scan. This imaging test uses X-rays and a computer to produce images (often called slices) of the body. A CT scan shows detailed images of any part of the body, including the bones, muscles, fat, and organs. CT scans are more detailed than general X-rays.
Magnetic resonance imaging (MRI). MRI uses a magnetic field, radio frequency pulses, and a computer to make detailed pictures of internal body structures. Sometimes injecting dye into a vein is used to produce images of body parts. The dye helps show the liver and other organs in the abdomen (belly).
How is alcohol-induced liver disease treated?
The goal of treatment is to restore some or all normal functioning to the liver.
You must completely stop drinking alcohol. This may involve an alcohol treatment program. Sometimes diet changes are advised, too. The liver is often able to repair some of the damage caused by alcohol so you can live a normal life. The scarring from cirrhosis is sometimes partially reversible, and when liver tissue loss is severe enough to cause liver failure, most of the damage may be permanent. However, the damage won't have any chance of reversing if you continue to drink alcohol.
Different treatments are needed for different complications and symptoms of alcoholic liver disease. For example, dietary modification, vitamins, salt restriction, procedures to shrink swollen veins in the digestive tract, water pills (diuretics), medicines to treat confusion, and antiinflammatory medicines.
In some cases, liver transplant may be considered. But you must complete a rehab program and go through alcohol detox before this is even an option.
What are the complications of alcohol-induced liver disease?
About one-third of people with alcohol-induced liver disease have hepatitis C virus. Others have hepatitis B virus. Your provider will test you for both and treat if needed. They are also at greater risk for liver cancer.
Nearly half have gallstones.
Those with cirrhosis often get kidney problems, intestinal bleeding, fluid in the belly, confusion, liver cancer, and severe infections.
Key points
Alcohol-induced liver disease is a common, but preventable, disease.
Alcohol-induced liver disease is caused by heavy use of alcohol. The liver breaks down alcohol. If you drink more than it can process, it can become seriously damaged.
The effects of alcohol on the liver depend on how much and how long you have been drinking.
The most important part of treatment is to completely stop drinking alcohol. Sometimes diet changes are advised, too.
The liver is often able to repair some of the damage caused by alcohol so the you can live a normal life. In some cases, liver transplant may be considered. But you must complete a rehab program and go through alcohol detox before this is even an option.
About one-third of people with alcohol-induced liver disease have hepatitis C virus. Others have hepatitis B virus. Your provider will test you for both and treat if needed. They are also at increased risk for liver cancer. Nearly half have gallstones. Those with cirrhosis often develop kidney problems, intestinal bleeding, fluid in the belly, confusion, liver cancer, and severe infections.
Next steps
Tips to help you get the most from a visit to your healthcare provider:
Before your visit, write down questions you want answered.
Bring someone with you to help you ask questions and remember what your provider tells you.
At the visit, write down the names of new medicines, treatments, or tests, and any new instructions your provider gives you.
If you have a follow-up appointment, write down the date, time, and purpose for that visit.
Know how you can contact your provider if you have questions.